Living with the symptoms of a sleep disorder can leave you feeling Beyond Tired®. Learn more from the NSF here.
This common sleep disorder can impact your ability to function during the day. Learn how to spot the symptoms and get the right treatment if you need it.
Insomnia—with all its tossing, turning, and nighttime disturbance—can wreak havoc on your sleep routine and the way you feel during the day. This disorder often prevents people from achieving the quality or quantity of sleep that their body needs to function at its best. The end result: daytime fatigue, as well as a decline in focus, concentration, and cognitive performance during waking hours. Learning the risk factors and symptoms associated with insomnia can help you understand ways to improve your sleep habits, plus when to seek professional help to find treatments for this challenging sleep disorder. No matter how long you may have had insomnia, effective treatment is available.
What Is Insomnia?
Insomnia is a sleep disorder that disturbs a person’s ability to fall asleep and/or stay asleep. You may wake up too early or struggle to return to sleep after awakening during the night. Approximately 40 million Americans experience insomnia every year and more than 57 percent of older adults experience a decline in quality of life and overall health due to insomnia. But while this sleep disorder is common, it’s also a complex condition that goes beyond experiencing an occasional sleepless night. Repeated occurrences can take a toll on your energy level, mood, productivity, and cognitive skills.
The two main types of insomnia are acute insomnia and chronic insomnia. Acute insomnia is short-term and often triggered by stressful life events. This form of insomnia typically resolves on its own without medical treatment. Chronic insomnia, a long-term and more serious form of the condition, occurs at least three nights per week for at least three months. Those suffering from chronic insomnia may find relief with lifestyle changes, cognitive therapy, or medical intervention.
Risk Factors for Insomnia
Insomnia sufferers don’t always have an underlying or coexisting condition that causes the sleep disorder. Still, there are certain factors that can make you more likely to experience recurring episodes of insomnia. For example, major life events such as the death of a loved one, job loss, divorce, illness, starting a new job, or moving may trigger stress that leads to insomnia. Women are also more prone to experience insomnia than men due to hormonal changes during their menstrual cycle, pregnancy, and menopause.
Other common risk factors for developing insomnia include:
- Chronic medical conditions and mental health disorders, such as asthma, gastroesophageal reflux disease (GERD), arthritis, depression, anxiety, allergies, and thyroid problems
- Taking certain medications
- Changes in sleep patterns and health as you get older
- Jobs with odd working hours, frequent travel, or changes in schedule
- Poor sleep habits and sleeping environment
- Excessive use of alcohol, caffeine, and nicotine
Look Out for These Symptoms
People with insomnia often complain about its effect on their ability to function during the day. Insomnia symptoms vary from person to person and can range from fatigue to anxiety, mood swings, and difficulty doing routine things. These are some of the common signs that you may have insomnia:
- Difficulty sleeping
- Waking up repeatedly or for long periods during the night
- Waking up too early
- Morning fatigue
- Moodiness, irritability, or depression
- Cognitive impairment
- Relationship problems
- Forgetfulness
- Increased errors or accidents
- Ongoing anxiety about sleep
If your symptoms worsen or persist over an extended period of time, talk with your healthcare provider about treatment options to address your insomnia symptoms.
Diagnosing Insomnia
Although there is no single definitive test to diagnose insomnia, your healthcare provider can use a variety of methods to determine the cause and impact of your sleep issues, rule out potential illnesses, and get to the root of the problem. A physical exam and blood test may also be used to determine if other coexisting medical conditions, medications and other substances, or underlying health issues are contributing factors to your sleep problems. It may help to keep a sleep diary to document your sleep patterns and symptoms for a few weeks. Your healthcare provider might suggest additional testing to determine if what appears to be insomnia is another type of sleep disorder.
How to Treat Insomnia
If you’ve tried to self-soothe your way back to sleep during a restless night, you’re not alone. Herbal tea, reading, listening to soft music, and even drinking alcohol are just a few of the tricks people may try to help themselves fall asleep. Self-medicating with alcohol, though, is unwise: It tends to disrupt sleep and causes long-term side effects.
If you tried following a healthy sleep routine, like NSF’s Best Slept Self® framework, but aren’t getting the insomnia relief you need, it’s time to talk to your healthcare provider about treatment options. Finding an insomnia treatment that works for you is crucial for your mental and physical health. Left untreated, insomnia can increase the risk of developing obesity, hypertension, depression, and other illnesses.
There isn’t a one-size-fits-all solution for treating insomnia. Some people will find relief through cognitive therapy and relaxation techniques, while others might need prescription medication to improve their sleep quality. Cognitive behavioral therapy for insomnia (CBT-I) works by helping patients identify and eliminate beliefs and behaviors that negatively affect their sleep. This treatment option also focuses on implementing strategies to develop good sleep habits and reduce excessive worrying that keeps you up at night.
Over-the-counter sleeping aids with sedating effects include the antihistamines diphenhydramine and doxylamine succinate, and supplements like melatonin and valerian root are available for short-term use.
Prescription sleeping pills are recommended for short-term or longer-term use, depending on the patient’s needs. Some options include:
- Benzodiazepine sedatives and non-benzodiazepine sedatives. These work to help people fall asleep. Examples of benzodiazepine sedatives are triazolam, estazolam, temazepam, flurazepam, and quazepam. Examples of non-benzodiazepine sedatives are zolpidem, eszopiclone, and zaleplon.
- Orexin receptor antagonists affect the action of the hormone orexin (chemicals involved in regulating the sleep-wake cycle) in the brain to help you sleep. Examples of orexin receptor antagonists include suvorexant and lemborexant.
- Low-dose doxepin works to block histamine receptors. It is intended for people who have trouble staying asleep to continue sleeping.
- Ramelteon is another insomnia medication that works differently than the other sedative medications by affecting melatonin receptors. It is designed specifically to help people fall asleep.
Many sleeping aids and medications can have side effects, such as daytime dizziness and grogginess. So make sure to talk with your healthcare provider about all the options, as well as any other medications that you might be taking, before making a treatment decision.
In summary, choosing safe and effective treatment options are key to managing insomnia. Start with some lifestyle changes, such as establishing a regular bedtime and reducing your caffeine intake later in the day so it doesn’t interfere with nighttime sleep. You might also benefit from creating a calm, relaxing sleep environment and eliminating distractions such as TV or texting on your phone before bed. As an additional step, you may want to talk to your healthcare provider about CBT-I and medication options. It can be a challenge to know exactly what’s causing your insomnia, but there are ways to help address it. Working with your healthcare provider to develop a personalized insomnia treatment plan can help you find the relief you need for a solid night’s sleep.
Contact: NSF Communications
703-243-1753
scorkett@thensf.org
National Sleep Foundation Highlights New Evidence for Screen Time Usage and Poor Sleep
Washington, D.C. (December 1, 2020): Featured in the December issue of the National Sleep Foundation’s (NSF) Sleep Health Journal, new research illuminates and reinforces the connection between poorer sleep and the amount of time children spend on screen media devices during the day.
Screen media use and sleep disturbance symptom severity in children (Garrett C. Hisler, Brant P. Hasler, Peter L. Franzen, Duncan B. Clark, Jean M. Twenge) sought to evaluate how screen media use relates to symptoms of sleep-wake disturbances. “Children who spend more time on screens have more trouble sleeping, while children who spend less time looking at screens each day fall asleep more quickly, sleep longer, have fewer sleep disturbances and insomnia symptoms, and are less sleepy during the day,” explained corresponding author Garrett Hisler, PhD, Postdoctoral Associate at the University of Pittsburgh.
“The results of this large study support the widespread understanding that screen-based media use is linked to delays and decreases in children’s sleep. As digital media devices have become more portable, children are more likely to bring a screen to bed with them, which not only delays bedtime, but may lead to sleep disruptions in the night,” said Lauren Hale, PhD, Professor at Stony Brook University and NSF Board Member. “More research is necessary to better understand how screen media effects on sleep health contribute to daytime consequences, including physical, psychological, and cognitive functioning,” Hale added.
Importantly, the authors concluded that screen use throughout the day affects sleep at night. NSF advises reducing evening screen time in children and adults for better sleep health. Phones can be psychologically stimulating and pose a barrier to falling asleep and staying asleep. Digital media devices have LED screens that emit blue light, which can affect the body’s natural sleep/wake cycle. Turning off electronic devices before bed and a relaxing wind-down routine lets the mind and body prepare for sleep. For information on how to help maintain good sleep health, see NSF’s Making Time for SLEEP.
About the National Sleep Foundation
The National Sleep Foundation (NSF) is a 501(c)3 nonprofit corporation dedicated to improving health and well-being through sleep education and advocacy. Founded in 1990, the NSF is committed to advancing excellence in sleep health theory, research and practice.
thensf.org │SleepHealthJournal.org
Feeling sleepy at night and awake during the day may seem like a given, but behind the scenes, a complex rise and fall of chemicals and hormones is involved. Learn how your body creates this natural rhythm.
Although it may seem straightforward that you sleep when you’re tired and wake when you’re rested, the mechanisms behind these behaviors are fairly complex. In fact, the strong urge to sleep isn’t necessarily dependent on how strenuous your day has been. Rather, your urge to sleep is guided by two factors: your sleep drive and your circadian rhythm. Sleep drive refers to a homeostatic system in your brain which makes you feel sleepy. With every hour that you are awake, your sleep drive gets stronger. The sleep/wake circadian rhythm is your body’s internal system that triggers both feelings of sleepiness that send you to bed and feelings of alertness that tell you it’s time to get up. Understanding how your sleep/wake rhythm works may help you get a better night’s sleep.
What Is a Circadian Rhythm?
Your circadian rhythm is the 24-hour cyclical ebb and flow of hormones and chemicals in your body that determine when you feel the need to go to sleep and get up. Most people need between seven and nine hours of sleep, followed by 15 to 17 hours of feeling awake. Your body and brain work together in multiple ways to create and regulate this process.
While 24 hours is the approximate length of the sleep/wake circadian rhythm, some people’s rhythms are slightly longer or shorter. In general, women have a circadian rhythm slightly shorter than 24 hours, and for this reason, they tend to be more “morning people.” Meanwhile, men typically have longer circadian rhythms and are more apt to be “night owls.”
The Role of the Brain
Inside the hypothalamus found in the brain is the suprachiasmatic nucleus (SCN) made up of 20,000 nerve cells. The SCN is sometimes referred to as the “master clock” because it plays an important role in the body’s daily rhythms. It receives input from the eyes, which is important since daylight and darkness play major roles in regulating the circadian rhythm. When light changes in the environment, the SCN signals to the body to produce larger or smaller amounts of different chemicals and hormones to influence how sleepy or awake you feel. For this reason, in winter months when days are shorter, you likely feel the urge to sleep sooner than in the summer when there is more sunlight. In places like Iceland where the sun never fully sets during peak summer days, blackout curtains or eye masks are helpful tools to help you sleep.
How Melatonin Works
One important hormone influenced by your SCN is melatonin, a chemical which makes you feel drowsy. In late afternoon as it gets darker out, your SCN tells the pineal gland in your brain to start releasing melatonin. The body’s level of this hormone begins to rise in response and continues to climb through the night. Melatonin levels begin to decline during the early morning as your body gets ready to wake up. Just as darkness is the signal that tells the body it’s time to release melatonin, bright lights can inhibit your body’s ability to produce this sleep-inducing hormone. Maintaining a dark bedroom at night and getting sunlight as soon as you wake can help you keep your melatonin levels in sync with your circadian rhythm.
Can You Change Your Circadian Rhythm?
Since your body’s sleep/wake rhythm is strongly influenced by exposure to light and its effect on your SCN, manipulating the amount of light in your space can affect your rhythm. If your schedule calls for an early-morning wakeup, exposing yourself to bright light, like sunlight, the instant the alarm goes off may help, since it encourages your SCN to release hormones that help you feel awake.
Living with the symptoms of a sleep disorder can leave you feeling Beyond Tired®. Learn more from the NSF here.
Loud snoring is only one of the signs of this serious sleep disorder. Learn the other symptoms and effects of sleep apnea and what your treatment options are.
Do you wake up in the morning feeling tired despite going to bed at a decent time and thinking you slept through the night? Has your partner told you that you were snoring all night?
If those situations sound familiar, you might be one of the millions of Americans suffering from sleep apnea, a serious medical disorder characterized by abnormal or interrupted breathing during sleep. Sleep apnea sufferers could experience hundreds of episodes of stopped breathing or irregular breathing each night. This disrupted sleep can cause fatigue throughout the day, leading to poor job performance as well as increasing the likelihood of car crashes and work-related accidents. Mental health can also suffer, leading to or increasing irritability, moodiness and depression. Sleep apnea can also put sufferers at increased risk for serious health issues including high blood pressure, cardiovascular conditions, stroke, Type 2 diabetes, liver problems, metabolic syndrome and complications with medications and surgery.
What Are the Two Forms of Sleep Apnea?
Obstructive sleep apnea (OSA) is the most common form of sleep apnea, and happens when the muscles in the back of your throat relax, causing the airway to narrow or close altogether when you breath in. Because this loss of air can reduce your blood oxygen level, your brain will send a signal to awaken you. Most sleepers won’t notice this sudden reaction although they could snort or choke for air in the process. These reactions can happen from five to 30 times or more per hour.
While loud snoring is a common symptom of obstructive sleep apnea (OSA), some sufferers of OSA don’t snore at all. However, they may experience other symptoms such as waking up with a dry mouth, daytime fatigue, headaches, irritability, lack of focus, night sweats, the frequent need to urinate, and sexual dysfunction.
Central sleep apnea, a less common form of apnea, is when your brain stops sending signals to your breathing muscles, stopping your breathing for short periods of time. These actions can make it more difficult to fall asleep or stay asleep. Sufferers might wake up with shortness of breath.
Regardless of the type of sleep apnea a person may have, the sleep disruptions they experience prevent them from reaping the health benefits of Stage 3 deep sleep, when muscle repair takes place and Stage 4 rapid eye movement (REM) sleep, which supports both short-term and long-term memory. That’s why a lack of deep and REM sleep can have significant negative consequences on long-term health.
Am I at Risk?
About 25 percent of men and 10 percent of women suffer from OSA (central sleep apnea is much less common). Risks increase for people over 50 and those who are overweight, but the condition can affect people of any age, including children. A family history of sleep apnea could increase your likelihood of developing sleep apnea. Existing medical conditions such as congestive heart failure, high blood pressure, Type 2 diabetes, stroke, Parkinson’s disease, polycystic ovarian syndrome, hormonal disorders, and chronic lung diseases such as asthma also can increase risk. Finally, the use of alcohol, tobacco, sedatives, narcotic pain medications, or tranquilizers could be connected with both types of sleep apnea.
How to Start Treatment
If someone in your home can watch you during sleep, have them observe your breathing patterns to see if you stop breathing or gasp for air, as those are signs of sleep apnea. If you are in fact experiencing these things, talk with your healthcare provider. They can schedule an evaluation with a sleep specialist, who can refer you for an overnight sleep study (officially known as a “polysomnogram”). This test will be done in a sleep center where a professional will measure your heart rate, breathing, air flow, blood oxygen, eye movements, and brain and muscle activity while you sleep. You’ll then receive a report about how often breathing stops or is disrupted during a typical sleep cycle. A home sleep test is another option that measures fewer functions but still can confirm a suspected sleep apnea diagnosis. Discuss with your healthcare provider to decide what might be best for you.
What Treatments Are Available?
If you’re diagnosed with OSA, depending on the severity of your condition, you might be able to treat it with a few lifestyle changes. Cutting back on alcohol, losing weight, and quitting smoking can help reduce sleep apnea. Sleeping on your side or stomach instead of on your back can also improve your breathing while asleep, and some might find relief through nasal sprays and breathing strips that cut down snoring and improve airflow. Your sleep specialist might also refer you to a dentist for a mouth appliance to keep the tongue in place or to adjust the jaw to keep the airway open during sleep.
Some patients with OSA or central sleep apnea may be treated using Continuous Positive Airway Pressure (CPAP) therapy, which involves wearing a mask over the nose and mouth while sleeping. These devices prevent your airway from closing by using air pressure to hold up airway tissues while you sleep. If CPAP isn’t effective for those with central sleep apnea, other breathing devices known as adaptive servo-ventilation (ASV) or bilevel positive airway pressure (BPAP) may be used. However, these are not recommended for people with heart failure, so be sure to talk with your healthcare provider about what might be right for you.
For cases that don’t improve through lifestyle changes or devices, surgery might be an alternative.
Common procedures that address OSA include surgeries to the nose, tongue, palate (soft tissue in the back of your mouth and throat) or the bones of your face, neck, and jaw. The aim of tongue surgery is to prevent the tongue from blocking the airway when it relaxes during sleep. There are several different palate surgeries and all aim to open or widen the airway. Common ones are tonsillectomy where large tonsils blocking the airway are removed and uvulopalatopharyngoplasty, or UPPP, where the throat’s tissue is surgically rearranged to create bigger airway. Skeletal surgery often involves changing the shape of the airway by moving the jawbone or partial removal of a bone in the chin and pulling the tongue and neck muscles forward to open up the airway.
Those with symptomatic heart failure who have central sleep apnea have a new surgical treatment option—the implantation of a nerve stimulator, similar to a pacemaker, in your chest. The device will stimulate your phrenic nerve to make you take a breath if it senses that you haven’t taken a breath in too long a period of time.
If you are experiencing any of the signs of sleep apnea, don’t disregard them. Talk to your healthcare provider for diagnosis and treatment. As part of Count On Sleep, NSF collaborates with the American Academy of Sleep Medicine and others on a CDC-funded awareness program to improve recognition of OSA. Learn from sleep medicine specialists how OSA is “More Than A Snore.”
Why do people snore? Is it okay to snore? Is there a way to stop it? Here’s what you should know about the common causes of snoring.
If your bed partner’s snoring sounds like a freight train, should you be concerned? While some may think the sound of snoring is funny or annoying, it can actually indicate a more serious health issue. That’s why it’s important to know the common causes of snoring, so you can do something about it if needed.
What Causes Snoring?
Snoring is the noise made by turbulent airflow. You don’t snore when you are awake, so what changes in sleep? When you sleep, the muscles in your throat lose tone and relax. Since your lungs stay the same size, you have to get the same volume of air through a smaller space. When air flows past your relaxed throat tissues and vibrates, the harsh, raspy noise that results is known as snoring. It can simply be caused by the anatomy of your mouth, throat, and sinuses. But snoring can also be due to a cold, allergies, alcohol consumption, being overweight, or sleeping on your back. Thirty-seven million people admit they snore regularly. More men (42%) than women (31%) say they are snorers.
Reasons for Snoring:
- The back of your throat—known as the soft palate—can narrow your airway if it’s low and thick. People who are overweight may also have narrowed airways. Additionally, having a long uvula—the triangle shaped piece of flesh hanging from the back of your throat—can obstruct air, causing snoring.
- Drinking alcohol before bed relaxes your throat muscles and may reduce airflow and increase vibration.
- A cold, sinus problem, or allergies can cause snoring by blocking air flow.
- Being overtired can cause the airways to relax more deeply, producing the noisy vibration.
- Sleeping on your back causes your airways to narrow due to gravity.
Are There Any Other Reasons People Snore?
Aside from those reasons mentioned above, some people become snorers as they age because their throat and tongue muscles weaken. Likewise, certain medications can relax those muscles and lead to snoring. Pregnant women may be prone to snoring towards the end of pregnancy, when hormones surge and cause nose tissues to swell. A crooked nasal septum or deviated septum— where the cartilage wall between the nostrils is off center—can also cause snoring.
When Is Snoring a Sign of Something More Serious?
Snoring may be linked with a sleep disorder called obstructive sleep apnea (OSA). Not everyone who snores has OSA, but if you have additional symptoms such as paused breathing during sleep, restless sleep, chest pain, gasping or choking at night, excessive daytime sleepiness, morning headaches, or memory problems, talk to your health care provider about your snoring.
What Can You Do About Snoring?
You can alleviate some causes of snoring with certain lifestyle changes. If, for example, you snore after having a glass of wine or two in the evening, try skipping it or drinking it earlier, and seeing if that works to end the snoring. If you carry excess weight, especially in the neck area, try losing weight to allow your airways to open up more. If you snore while sleeping on your back, try changing sleep positions or raising your head on a pillow.
If none of these changes seems to work or your snoring gets louder or more frequent, talk with your healthcare provider, who can evaluate your symptoms and may order a home sleep test (HST) or an overnight laboratory sleep study for further analysis. They can also examine whether the anatomy of your mouth, throat, or nasal septum might be causing your snoring. If so, surgery may be another option. Again, talk with your healthcare provider to explore the best possible approach for you.
Since snoring sometimes has negative health consequences, don’t just laugh it off. If you or your bed partner is a chronic snorer, find out if it’s a sign of a more serious medical condition and get the treatment you may need.
Your eating habits can be crucial for quality sleep. Learn how your food choices and your meal timing can make a difference.
There’s a connection between nutrition and sleep.
For example, diets low in fiber and high in saturated fat may decrease the amount of deep, restorative sleep you’ll get. Excess sugar can cause you to awaken more frequently. Consuming certain foods and beverages close to bedtime can also lead to poor sleep.
If you’re having trouble falling and staying asleep, the culprit could be what you’re choosing to eat and drink.
What to Avoid
Fatty or high-protein foods: Because digestion naturally slows when you sleep, going to bed too soon after eating a steak dinner or other high-protein foods can lead to disrupted sleep, since your stomach will feel uncomfortably full. Foods high in saturated fat have a similar disruptive effect on sleep patterns.
Spicy foods: Spicy foods can cause painful heartburn that could make it difficult to lie down comfortably, which makes it harder to fall asleep. Heartburn can also worsen the effects of obstructive sleep apnea (OSA), as the backed-up acid can create more irritation in your airway. Some spicy foods can raise your body temperature, forcing your body to work harder to cool down enough to fall asleep; feeling too warm in bed may also disrupt your sleep patterns throughout the night.
Caffeine: Drinking caffeine late in the day has long been known as a potential sleep disrupter for many people, since it’s a stimulant designed to keep you alert. But be aware that caffeine can be hidden in other foods as well, such as chocolate and even ice cream, so check the ingredients.
Alcohol: Winding down with a glass of wine or a beer at dinner can be a pleasurable experience, but not so much when you’re getting ready to sleep. Once the effects of alcohol wear off, you’ll likely find yourself waking suddenly and struggling to go back to restful sleep. Alcohol can also worsen OSA symptoms.
Go ahead and enjoy flavorful foods and drinks, but note that fatty and high-protein foods and alcohol close to bedtime can affect your sleep, so consume them in moderation. And cutting off caffeine in the afternoon is a good idea since caffeine’s effects can last up to six hours, and sometimes even longer if the beverage is high in caffeine.
What to Choose Instead
If you need a snack before bedtime, consider complex carbohydrates such as oatmeal or whole-wheat toast, which digest easily.
Healthy eating habits overall will encourage healthier sleeping patterns. Consuming a high-fiber diet with fresh fruits, vegetables, whole grains, and low-fat proteins—while avoiding foods with added sugars—is ideal. Look for foods high in B vitamins; B vitamins are believed to help regulate melatonin. Foods rich in B vitamins include fish, lean poultry and meat, legumes, eggs, and dairy.
A healthy diet can also help you lose weight, which can in turn lead to better sleep and make you less likely to suffer from daytime fatigue, insomnia, and OSA.
The takeaway? Good eating habits can go hand in hand with getting a good night’s sleep for a healthier you.
When the lights go out, your body’s sleep cycle is only just beginning. Learn what you need to know about the sleep stages.
Sleeping may seem like a passive activity. However, as you’re peacefully asleep in your bed, your body is cycling through four stages that serve specific purposes. Learn about the different sleep stages and how a normal sleep cycle works.
What Is a Sleep Cycle?
While scientists in the 1950s thought that your brain went into “shutdown” mode while you slept, we now know that your sleeping body cycles through regular sleep patterns of activity, known as the sleep cycle. Over the course of one night, your body goes through the sleep stages every 90 minutes or so. Sleep stages last for different periods of time depending on the age of the sleeper.
The first three sleep stages are categorized as non-REM sleep, and the fourth and final sleep stage is Rapid Eye Movement (REM) sleep.
Stage 1
Stage 1 of the sleep cycle is the lightest phase of sleep and generally lasts about seven minutes. The sleeper is somewhat alert and can be woken up easily. During this stage, the heartbeat and breathing slow down while muscles begin to relax. The brain produces alpha and theta waves.
Stage 2
In Stage 2, the brain creates brief bursts of electrical activity known as “sleep spindles” that create a distinct sawtooth pattern on recordings of brain activity. Eventually, the waves continue to slow down. Stage 2 is still considered a light phase of sleep, but the sleeper is less likely to be awakened. Heart rate and breathing slow down even more, and the body temperature drops. This stage lasts around 25 minutes.
Stage 3
This stage represents the body falling into a deep sleep, where slow wave sleep occurs. The brain produces slower delta waves, and there’s no eye movement or muscle activity from the sleeper. As the brain produces even more delta waves, the sleeper enters an important restorative sleep stage from which it’s difficult to be awakened. This phase of deep sleep is what helps you feel refreshed in the morning. It’s also the phase in which your body repairs muscle and tissue, encourages growth and development, and improves immune function.
REM Sleep
About 90 minutes after falling asleep, your body enters REM sleep, which stands for Rapid Eye Movement sleep and is named so for the way your eyes quickly move back and forth behind your eyelids. REM sleep is thought to play a role in central nervous system development in infants, which might explain why infants need more REM sleep than adults. This sleep pattern is characterized by dreaming, since your brain is very active during this stage. Physically, your body experiences faster and irregular breathing, increased heart rate, and increased blood pressure; however, your arm and leg muscles become temporarily paralyzed, stopping you from acting out your dreams. REM sleep increases with each new sleep cycle, starting at about ten minutes during the first cycle and lasting up to an hour in the final cycle. Stage 4 is the last stage before the cycle repeats. This sleep stage is critical for learning, memory, daytime concentration, and your mood.
While all sleep stages are important, Stage 3 and REM sleep have unique benefits. One to two hours of Stage 3 deep sleep per night will keep the average adult feeling restored and healthy. If you’re regularly waking up tired, it could be that you’re not spending enough time in that deep sleep phase. Meanwhile, REM sleep helps your brain consolidate new information and maintain your mood – both critical for daily life. Talk to your health care provider if you feel you are not getting the restful sleep that you need.
If you’re having trouble getting a good night’s sleep, it could be that your bedroom isn’t set up optimally. Use these four tips to help create a relaxing, sleep-friendly bedroom.
Late night TV, smartphone on the nightstand, laptop left open across the room—while these might be found in your average bedroom at night, they could actually be hurting your sleep quality. Make a few simple changes to your bedroom with these four tips and create a better sleep environment.
Darken Your Room
Light slows the production of melatonin, a naturally-occurring hormone that promotes sleep. That’s why keeping your bedroom dark is an essential part of creating a good sleep environment.
Dim the lights in your room as bedtime approaches to signal to your brain that it’s time to wind down for the night. Also reduce your blue light exposure—turn off electronics with screens like TVs and computers and set your smartphone to “nighttime” settings—continued exposure to this light can keep you awake even if you have your room lights turned off. To make sure your bedroom stays dark throughout the night, be sure to lower your shades or use blackout curtains.
Lower the Temperature
As you fall asleep, your body temperature naturally decreases to promote the sleep-inducing process. Keeping your bedroom cool facilitates this natural occurrence and makes it easier for you to fall asleep and stay asleep.
Optimal sleep temperature is slightly different for everyone, so experiment with different nighttime temperature settings in your search for a good sleep environment. In general, experts consider 60 to 67 degrees to be optimal for high quality sleep.
Choose a Comfortable Mattress and Sheet Set
Identifying what type of mattress, sheets, and pillows are most comfortable to you is important for a night of restful sleep.
Your mattress preference might depend on your sleep position, whether you share a bed, if you tend to “run hot” when you sleep, and other factors. A comfortable pillow will help support your neck and back throughout the night; a poorly chosen pillow, on the other hand, can contribute to headaches, neck pain, and arm numbness.
Also consider what you put on top of your mattress. Choosing a mattress cover or sheet set that feels pleasant will make it easier to fall asleep and decrease the likelihood that you wake up during the night from being too hot or too cold. Test out the feel of different sheets or blankets to determine which one you like best, then select your favorite ones.
Reduce Noise
Minimizing noise in the bedroom at night can increase the amount of deep sleep you get while also making it less likely that you’ll wake up during the night. When it’s time for bed, turn off all outside sounds (including the TV—the sudden changes in volume make it harder for you to fall and stay asleep). A quiet environment is much more conducive to a peaceful night of sleep.
If you live on a busy street or have a neighbor who stays up late practicing guitar, consider products that help to reduce or mask distracting noise. Try a white noise machine and try to position your bed away from shared walls or street-facing windows.
By setting up your bed in a way that’s most comfortable for you, and keeping your room dark, cool, and quiet, you’ll be able to transform your bedroom into a sleep environment that promotes restful nights.
Healthy sleep is critically important for your productivity and safety at work. Learn how SleepWorks® for you on and off the job.
Is it bad if you only log four, five, or six hours of sleep a night? Watch out for these signs that you need more sleep.
Some people claim they only need five or six hours of sleep per night. However, the National Sleep Foundation’s 2015 landmark guidelines recommend that adults 18 to 64 get seven to nine hours of sleep nightly; for adults 65 and over, seven to eight hours nightly is best.
What Causes Lack of Sleep?
Many different factors can cause you to get less than five or six hours of sleep per night, such as being stressed or worried, eating a big meal too close to bedtime, drinking alcohol in the evening, or consuming caffeine too late in the afternoon. There are other contributors that may not be as obvious, such as:
Age: People 65 or over can tend to have more trouble sleeping due to natural circadian body clock changes as we age, medications or health problems.
Illness: Common conditions such as depression, anxiety, pain, cancer, and Alzheimer’s disease can all interfere with sleep. Lung, heart, kidney, and urological diseases can also cause sleep disturbances.
Sleep disorders: Insomnia, obstructive sleep apnea, and restless leg syndrome can be responsible for keeping you awake.
Other causes: Poor sleep habits, such as a lack of a consistent bedtime routine or not going to bed and getting up at the same time daily, can result in a lack of quality sleep. A change in schedule, noise, and other disruptions in your sleep environment can also play a role.
Signs You’re Not Getting Enough Sleep
If you’re sleeping less than what your body needs, you may experience symptoms in addition to feeling tired, such as:
- Inability to concentrate
- Difficulty with memory
- Puffy eyes, bags, or dark circles under eyes
- Feeling hungrier or gaining weight
- Irritability or moodiness
- Depression
- Increased bouts with illness
Continued lack of sleep can increase your risk for serious health conditions like high blood pressure, heart disease, stroke, and mental illness, as well as increase the likelihood of workplace mistakes and car crashes. That’s why it’s so important to address sleep problems as quickly as possible with the aim of improving the length and quality of your sleep.
How to Get the Recommended Amount of Sleep
What can you do to get the recommended amount of sleep? Put parameters on your screen time—shut off your computer and put down your smartphone at least an hour before bed and keep them outside of your bedroom if possible—artificial light from screens suppresses melatonin, the hormone that helps you feel sleepy.
Also, while watching TV before bed may seem relaxing, it can actually be too stimulating. Instead, do something truly calming like listening to a podcast or music, or reading a book. Skip heavy meals and caffeine, and limit alcohol to one drink.
Other healthy habits that promote good sleep are eating nutritious foods, exercising, maintaining a healthy weight, and setting up your bedroom so it’s an optimal environment for sleep. Doing these things should help you get the recommended number of hours of sleep each night.
Healthy sleep is crucial for your productivity and safety at work. Learn how SleepWorks® for you on and off the job.
Being a diligent driver starts with being aware – drowsy driving is preventable.
Sleepiness can slow down your reaction time, decrease awareness, impair judgment, and increase your risk of crashing. Whenever you are getting ready to drive, ask yourself, “Am I alert enough to operate a 3,000-pound fast-moving machine on public roads?”
Before getting into the car with someone or driving yourself, ask the following:
- Are you sleep-deprived or fatigued? Are you suffering regularly from sleep problems? Less than 6 hours of sleep triples your risk of falling asleep while driving!
- Are you planning to drive long distances without proper rest breaks?
- Will you be driving through the night, mid-afternoon, or when you would normally be asleep?
- Are you taking medications that can make you sleepy such as antidepressants, cold tablets, or antihistamines?
- Have you been working for more than 60 hours a week? A tightly packed work schedule increases your risk of drowsy driving by 40%.
- Have you been working more than one job and your main job involves shift work?
- Did you drink alcohol? Even a small amount of alcohol can have an impact on your body.
Be proactive. Plan every short and long trip ahead of time. Ask a friend to join you on long-distance drives, so that your companion can help look for early warning signs of driver fatigue and switch drivers when needed.
8 Drowsy Driving Warning Signs to Watch for:
- Finding it hard to focus on the road, frequent blinking, or heavy eyelids
- Starting to daydream, wandering eyes, and have disconnected thoughts
- Having trouble remembering the last few miles driven
- Missing an exit or ignoring traffic signs
- Yawning repeatedly or rubbing your eyes
- Finding it hard to keep your head up or nodding off
- Drifting from your lane, tailgating, or hitting a shoulder rumble strip
- Feeling restless and irritable, or becoming aggravated with common annoyances such as sitting in traffic.
If you notice any of these drowsy driving warning signs, pull over to a safe place and get some rest, stretch, or drink a caffeinated beverage. Continue driving when you feel alert and refreshed.
For more information about drowsy driving, visit the Drowsy Driving Prevention Week page to learn more.
For Immediate Release
Contact: NSF Communications
703-243-1753
scorkett@thensf.org
Choose Sleep First. Drive Alert. Drowsy Driving Prevention Week® 2020
WASHINGTON, DC, November 1, 2020 — The National Sleep Foundation (NSF) announces November 1-8 as Drowsy Driving Prevention Week® for 2020.
Drowsy driving is responsible for more than 6,400 U.S. deaths annually and is a public health concern. NSF’s annual campaign goal is to reduce the number of drivers who drive while sleep deprived.
“Fall-asleep crashes are often caused by choosing to drive without getting enough sleep. NSF encourages everyone to prioritize sleep and drive when alert and refreshed,” said NSF Chair, Dr. Richard Bogan.
Three key steps before driving can help prevent falling asleep behind the wheel:
- getting the recommended amount of sleep the night before your trip (7-9 hours on average),
- planning long trips with a companion, and
- scheduling regular stops every 100 miles or 2 hours.
The NSF Drowsy Driving Consensus Working Group’s 2016 report published in Sleep Health Journal concluded that sleep deprivation renders motorists unfit to drive a motor vehicle. Specifically, healthy drivers who have slept for two hours or less in the preceding 24 hours are not fit to operate a motor vehicle. NSF experts further agreed that most healthy drivers would likely be impaired with only 3 to 5 hours of sleep during the prior 24 hours.
Join NSF to help prevent drowsy driving. Access educational resources today on www.thensf.org and share the campaign’s message on social media using the hashtag #Sleepfirst.
—
About the National Sleep Foundation
The National Sleep Foundation (NSF) is a 501(c)3 nonprofit corporation dedicated to improving health and well-being through sleep education and advocacy. Founded in 1990, the NSF is committed to advancing excellence in sleep health theory, research and practice.
thensf.org │SleepHealthJournal.org
For Immediate Release
Contact: NSF Communications
703-243-1753
scorkett@thensf.org
National Sleep Foundation Highlights Racial Discrimination as a Component of Insomnia Severity
Washington, D.C. (October 19, 2020): The latest issue of the National Sleep Foundation’s (NSF) Sleep Health Journal highlights research that describes how racial discrimination is a contributor to worsened severity of insomnia among people of color with insomnia.
“Our findings show that racial discrimination is a potential explanation for why people from racial minority groups experience more severe insomnia symptoms” explained lead author Philip Cheng, PhD, Henry Ford Health System.
Some past research on racial differences in sleep disorders has shown that Caucasian patients experienced worse severity of insomnia than Black patients. “The current study was born out of the observation that in the research field, insomnia is thought of as a physiological process. It is easy to forget there are psychosocial factors that can contribute to a sleep disorder, which include environment and interactions within the environment. This is why racial discrimination was important to investigate and identify as a potential contributor in worsening sleep disorders,” explained Cheng.
“This paper makes a point of studying the connection between severe insomnia and social determinants of health, specifically racial discrimination. Publishing research that helps us better understand possible social determinants of sleep health is a primary goal of our journal. This research provides new insights on how and why people of color’s experience of discrimination can have negative effects on sleep and health,” said Orfeu Buxton, PhD, Editor-in-Chief of Sleep Health and professor of Biobehavioral Health at Pennsylvania State University.
About the National Sleep Foundation
The National Sleep Foundation (NSF) is a 501(c)3 nonprofit corporation dedicated to improving health and well-being through sleep education and advocacy. Founded in 1990, the NSF is committed to advancing excellence in sleep health theory, research and practice.
thensf.org │SleepHealthJournal.org
For Immediate Release
Contact: NSF Communications
703-243-1753
scorkett@thensf.org
Drowsy Driving Prevention Week® 2020
WASHINGTON, DC, October 13, 2020 – Today, the National Sleep Foundation (NSF) announces that Drowsy Driving Prevention Week® 2020 will be November 1-8.
NSF’s annual campaign goal is to reduce the number of drivers who elect to drive while sleep deprived. Drowsy driving is responsible for more than 6,400 U.S. deaths annually. Fall asleep crashes are often caused by voluntarily not getting the sleep you need. NSF encourages everyone to prioritize sleep and drive when alert and refreshed.
NSF invites transportation, safety and hospitality companies to promote drowsy driving prevention November 1 to 8.
NSF’s drowsy driving prevention resources, such as graphics and social media materials, will be available on www.thensf.org on October 22. NSF encourages spreading the word on Drowsy Driving Prevention Week through social media using hashtag #Sleepfirst.
—
About the National Sleep Foundation
The NSF is dedicated to improving health and well-being through sleep education and advocacy. Founded in 1990, the NSF is committed to advancing excellence in sleep health theory, research and practice.
For Immediate Release
Contact: NSF Communications
703-243-1753
scorkett@thensf.org
Itamar Medical Wins National Sleep Foundation 2020 SleepTech® Award
Washington, D.C. (October 5, 2020): The National Sleep Foundation (NSF) named Itamar Medical Ltd. (NASDAQ and TASE: ITMR) winner of the 2020 SleepTech® Award. The SleepTech® Award recognizes the year’s most innovative efforts in advancing sleep technology.
Itamar Medical is a technology company focused on the development and commercialization of non-invasive medical devices and solutions to aid in the diagnosis of respiratory sleep disorders. Itamar Medical describes its WatchPAT™ ONE as the first and only disposable home sleep apnea test that connects to a smartphone app and easily transmits sleep data for review.
“We congratulate Itamar Medical for winning our 2020 SleepTech Award by further innovating their product to help advance sleep technology. Their response to customer insights and needs is particularly relevant this year in the effort to promote better sleep health during a pandemic,” said John Lopos, CEO of NSF.
“We are honored and delighted to receive the 2020 SleepTech® Award and to be recognized by the NSF for our achievements in the field of sleep medicine and technology. Sleep Apnea is a serious disease with serious consequences. We are very proud of the home-based innovative technology and the digital health platform we have built to deliver simple and reliable solutions for the diagnosis and management of this condition,” said Gilad Glick, CEO, Itamar Medical.
The NSF would also like to acknowledge two semi-finalists: EnsoData and Bryte. EnsoData’s EnsoSleep is a sleep scoring AI technology, which reads waveforms to diagnose, monitor, and treat patients. Bryte’s Restorative Bed measures, learns, tests, and applies what sleepers need to improve their sleep. “We couldn’t have been more impressed with all three finalists. We struggled to select a winner,” said judge Lloyd Sommers, Chair of the NSF Sleep Tech Council.
The SleepTech® Award is given annually by NSF based on the recommendation of a panel of sleep experts who review the descriptions and representations of how the applicants’ products and services support sleep science and achieve innovation in sleep technology in order to improve sleep health.
NSF has no financial relationship with the 2020 SleepTech Award winner.
—
About the National Sleep Foundation: National Sleep Foundation (NSF) is a 501(c)(3) nonprofit corporation dedicated to improving health and well-being through sleep education and advocacy. Founded in 1990, the NSF is committed to advancing excellence in sleep health theory, education, research and practice. theNSF.org │SleepHealthJournal.org
Getting enough sleep is doable and important for your health. Read on for how many hours to strive for at every age.
Sleep is essential to feeling rested and alert. Getting the right amount for your mind and body feels great and helps you wake up feeling refreshed and ready to go. Every person is different when it comes to the exact amount of sleep that’s optimal for them, but most people fall within a range, depending on their age. These guidelines can help you determine how much sleep you really need, while providing some easy ways to achieve it.
How Many Hours of Sleep Do You Need?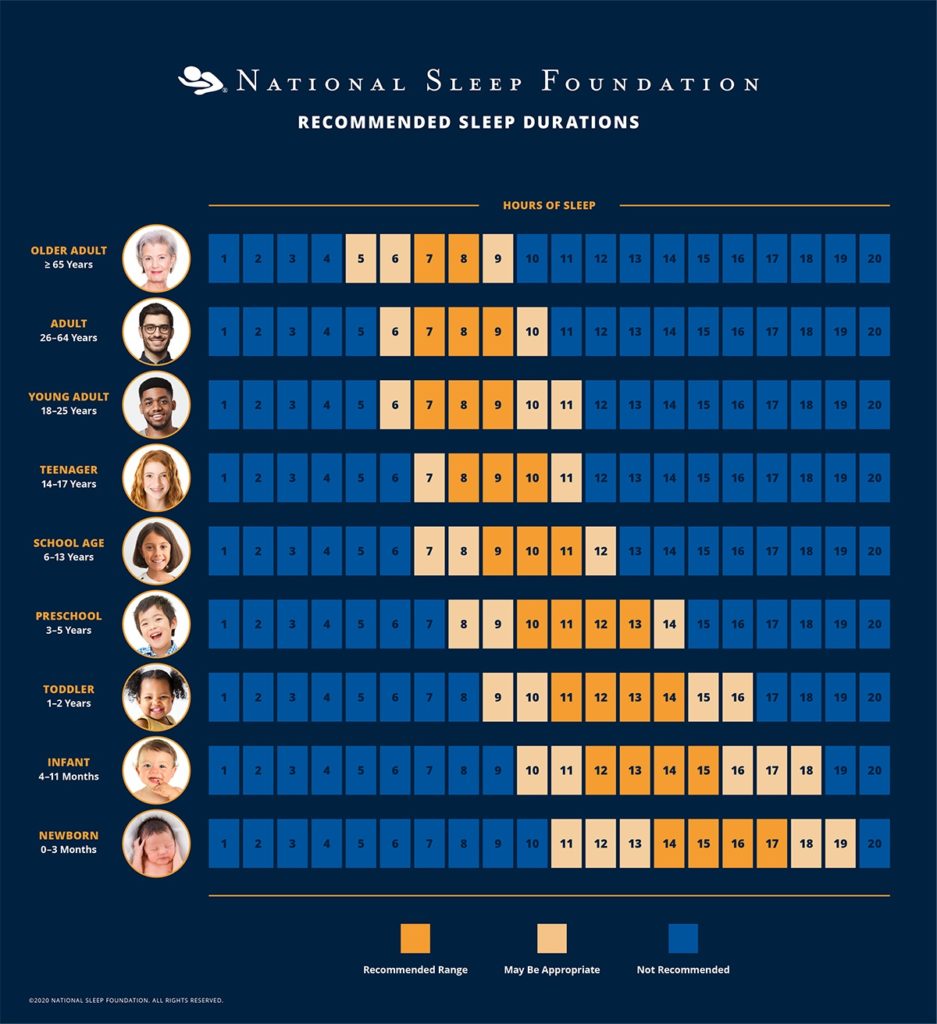
There is no precise number of minutes or hours of sleep at night that guarantees you will wake up feeling totally refreshed. But based on your age and lifestyle, what’s recommended for you likely falls within a certain range. To help yourself stay alert during the day, try sticking with these guidelines.
Newborns: From 0-3 months, babies need between 14 and 17 hours of sleep. This includes daytime naps, since newborns rarely sleep through the night. Older infants (4-11 months) need about 12 to 15 hours of sleep each day.
Toddlers: Between the first and second year of life, toddlers need between 11 and 14 hours of sleep each night.
Children: Preschoolers (3-5 years) should get 10 to 13 hours, while school-age kids (6-13 years) should strive for nine to 11 hours each night.
Teenagers: As kids get older, their need for sleep decreases slightly. Teens (14-17 years) require about eight to 10 hours of nightly sleep.
Adults: Between the ages of 18 and 64, adults should aim for seven to nine hours of nightly sleep. If you’re older than 65, you may need a little less: seven to eight hours is recommended.
Build in Some Flex Time
Some people can function well on the lower end of the range and others will need every minute of the upper limit. In fact, an additional hour or two on either side of a given range may be appropriate, depending on the person. Still, straying too far from the recommended amount could lead to a variety of health issues. For example, shortchanging sleep has been associated with weight gain, reduced immunity, high blood pressure, and depression.
The negative effects of too little or too much sleep aren’t just physical—they can also interfere with your mental health. Your outlook, mood, and attention span all depend on getting the right amount of sleep, and without it, your job performance (not to mention your personal life) can suffer.
Easy Ways to Get More Sleep
If getting enough sleep seems like an uphill battle, there are a few tips you can try. To start, head to bed at the same time every night, to allow your body to settle into a regular sleep-wake schedule. Just the way kids benefit from a set schedule, adults who stick to a regular pre-sleep routine that includes reading, meditation, journaling, and a warm bath may find it easier to wind down in the evening.
To help get quality sleep, avoid alcohol, caffeine, and spicy and fried foods right before bedtime. Aim for a bedroom temperature between 60 and 67 °F, make sure it’s dark, and block any bothersome noises with a pair of earplugs. For a fuller list of sleep tips, read them here.
For Immediate Release
Contact: NSF Communications
703-243-1753
scorkett@thensf.org
National Sleep Foundation Highlights New Evidence for Sleep Health Disparities
Washington, D.C. (September 24, 2020): The latest issue of the National Sleep Foundation’s (NSF) Sleep Health Journal features a collection of new research studies that add to the evidence base for racial, ethnic, and socioeconomic disparities in sleep health.
“The mission of Sleep Health is to explore sleep’s role in population health and elucidate the social science perspective on sleep and health. Sources and consequences of sleep disparities are central to this mission, and multiple new manuscripts in the latest issue illuminate a broad range of factors that can contribute to sleep disparities,” said Orfeu Buxton, PhD, Editor-in-Chief of Sleep Health and professor of Biobehavioral Health at Pennsylvania State University.
The August 2020 issue (Vol. 6, Issue 4) includes seven studies in which social factors were shown to be associated with sleep health disparities:
Police stops and sleep behaviors among at-risk youth (Dylan B. Jackson, PhD, Alexander Testa, PhD, Michael G. Vaughn, PhD, and Daniel C. Semenza, PhD)
Racial differences in sleep duration intersect with sex, socioeconomic status, and U.S. geographic region: The REGARDS study (Megan E. Petrov, PhD, D. Leann Long, PhD, Michael A. Grandner, PhD, Leslie A. MacDonald, ScD, Matthew R. Cribbet, PhD, Rebecca Robbins, PhD, Jenny M. Cundiff, PhD, Jennifer R. Molano, MD, Coles M. Hoffmann, MA, PhD, Xuewen Wang, PhD, George Howard, DrPH, and Virginia J. Howard, PhD)
Hispanic/Latino heritage group disparities in sleep and the sleep-cardiovascular health relationship by housing tenure status in the United States (Symielle A. Gaston, PhD, MPH, Selena Nguyen-Rodriguez, PhD, MPH, Allison E. Aiello, PhD, MS, John McGrath, MA, W. Braxton Jackson, II, MPH, Anna Nápoles, PhD, MPH, Eliseo J. Pérez-Stable, MD, and Chandra L. Jackson, PhD, MS)
Maternal experiences of racial discrimination and offspring sleep in the first 2 years of life: Project Viva cohort, Massachusetts, USA (1999-2002) (Chloé A. Powell, MD, Sheryl L. Rifas-Shiman, MPH, Emily Oken, MD, MPH, Nancy Krieger, PhD, Janet W. Rich-Edwards, ScD, Susan Redline, MD, MPH, and Elsie M. Taveras, MD, MPH)
Associations between self-reported sleep duration and cardiometabolic risk factors in young African-origin adults from the five-country modeling the epidemiologic transition study (METS) (DE Rae, LR Dugas, LC Roden, EV Lambert, P Bovet, J Plange-Rhule, T Forrester, W Riesen, W Korte, SJ Crowley, S Reutrakul, and A Luke)
Understanding sleep facilitators, barriers, and cultural dimensions in Native American urban youth (Alina I. Palimaru, PhD, MPP, Ryan A. Brown, PhD, MA, Wendy M. Troxel, PhD, MS, Daniel L. Dickerson, DO, MPH, Carrie L. Johnson, PhD, and Elizabeth J. D’Amico, PhD, MA)
Sleep deprivation in an American homeless population (Ariana Gonzalez, OTD, OTR/L, and Quinn Tyminski, OTD, OTR/L)
“At different times in its 30-year history, NSF has explored associations between socio-demographic factors and sleep. With Sleep Health, we are ensuring more than ever that today’s scientists and scholars have a rigorous platform to share findings that can help the public,” said John Lopos, CEO of NSF.
“This collection of research centered around sleep health disparities demonstrate the importance of focusing on the wide range of modifiable environmental and sociocultural determinants of health across the life course, which can be considered manifestations of addressable social ills such as structural racism,” said Chandra Jackson, PhD, MS, Research Investigator at the National Institutes of Health and Associate Editor of Sleep Health.
NSF is committed to using Sleep Health as an outlet for information and insight to help reduce racial and other disparities in sleep health and well-being. Sleep Health continues to feature research that seeks to explain these disparities, identify predictors, and present evidence that can be translated into changes that increase opportunities for improved sleep heath.
About the National Sleep Foundation
National Sleep Foundation (NSF) is dedicated to improving health and well-being through sleep education and advocacy. Founded in 1990, the NSF is committed to advancing excellence in sleep health theory, research and practice.
theNSF.org │SleepHealthJournal.org
Contact NSF Communications
703-243-1753
scorkett@thensf.org
National Sleep Foundation Partners with Samsung to Provide Sleep Health Education
Washington, D.C. (August 5, 2020): Today, the National Sleep Foundation (NSF) announced a partnership with Samsung Electronics Ltd to provide millions of Samsung device users with sleep health education and tailored information on the Samsung Health app, available on the new Galaxy Watch3, released today.
Samsung’s new Galaxy Watch3 will feature an updated sleep tracking function that will generate a “sleep score” within the Samsung Health app. Users’ sleep scores will be accompanied by NSF educational sleep health messages.
“Samsung has been evolving its sleep management offering since its introduction in 2014. Now, we are excited to take it to the next level by working with a leading sleep expert, the National Sleep Foundation, to provide users with a deeper understanding of their sleep,” said Taejong Jay Yang, Corporate SVP and Head of Health Team, Mobile Communications Business at Samsung Electronics. “And, when combined with the broad range of health and fitness metrics available in Samsung Health, users can get better insight into their overall well-being to help them feel their best selves.”
“We are enthusiastic to collaborate with a global technology leader like Samsung to reach millions of people across the world with sleep health information,” said National Sleep Foundation CEO John Lopos. “Samsung is making another commitment to its users by involving NSF as they look to advance the sleep health through their devices. NSF’s mission is to improve the sleep health and well-being of the public and this work is one way to help us achieve that goal.”
As technology and health become more intertwined, NSF plans to partner with industry leaders like Samsung to reach more consumers and achieve the organization’s sleep health mission. For more information on industry partnerships, please visit thensf.org/sleep-tech.
About the National Sleep Foundation
The National Sleep Foundation (NSF) is a 501(c)3 nonprofit corporation dedicated to improving health and well-being through sleep education and advocacy. Founded in 1990, the NSF is committed to advancing excellence in sleep health theory, research and practice.
thensf.org │SleepHealthJournal.org
###
For Immediate Release
Contact: NSF Communications
703-243-1753
scorkett@thensf.org
National Sleep Foundation Announces Board of Directors
Washington, D.C. (July 9, 2020): Richard K. Bogan, MD, will continue his role as Chair of the National Sleep Foundation board of directors in FY21. Dr. Bogan is the President of Bogan Sleep Consultants, LLC, and a Medical Officer of SleepMed, Inc., the largest sleep diagnostic company in the United States. He is also Associate Clinical Professor at the University of South Carolina School of Medicine and Associate Clinical Professor at the Medical University of South Carolina in Charleston, SC. Dr. Bogan has served as principal investigator on numerous clinical trials and has a variety of publications and research interests that focus on topics such as narcolepsy, insomnia, sleep apnea, shift work sleep disorder, restless legs syndrome, chronic fatigue/fibromyalgia and circadian rhythm abnormality. As Chair of the National Sleep Foundation, Dr. Bogan will continue to lead a board of directors composed of physicians, scientists, and business professionals.
“It’s an honor to continue to serve as the Chair of the National Sleep Foundation board of directors. We have an important mission and role as the global voice for sleep health. I look forward to an exciting year of new programs and initiatives to improve sleep health,” said Bogan.
Also starting July 1, Lauren Hale, PhD, will serve as Vice Chair. Dr. Hale is Professor of Preventive Medicine, Program in Public Health, at SUNY, Stony Brook. Benjamin Gerson, MD, Thomas Jefferson University, will serve as Treasurer, and David N. Neubauer, MD, Associate Director of the Johns Hopkins Sleep Disorders Center, will serve as Secretary. Other members of the board include Helen Chang, RPh, Thomas DiSalvi, CDS, Paul P. Doghramji, MD, Jerrold A. Kram, MD, Steven E. Lerman, MD, MPH, Maurice M. Ohayon, MD, DSc, PhD, Temitayo Oyegbile, MD, PhD, Rafael Pelayo, MD, Kristen E. Prinz, JD, and Desmar Walkes, MD.
Stephen Sheldon, DO has completed his term on the NSF board of directors. NSF thanks Dr. Sheldon for his years of service to NSF and his continued support of NSF’s mission.
—-
About the National Sleep Foundation
National Sleep Foundation (NSF) is a 501(c)3 nonprofit corporation dedicated to improving health and well-being through sleep education and advocacy. Founded in 1990, the NSF is committed to advancing excellence in sleep health theory, research and practice.
theNSF.org │SleepHealthJournal.org
The National Sleep Foundation (NSF) exists to help improve the sleep health and well-being of the public. We embrace and celebrate differences among us and understand that we are all connected by our shared fundamental human needs and rights. NSF can never accept beliefs or behaviors that foster racism, fuel hate, risk public safety, or restrict equal opportunities for everyone to thrive. To this end, we stand with the Black community and all communities that have endured unequal treatment, and we will affirm our commitment by:
- Increasing our commitment to diversity across our Board of Directors, Staff, and Volunteers
- Fortifying our government affairs and policy agenda to include the sleep health needs of the Black community, other communities of color, and historically underserved groups of people
- Committing to continue to use our journal Sleep Health as a rigorous source of information and insight to help solve racial and other disparities that exist in sleep health and well-being
- Exploring new, transformational opportunities to help improve sleep health and well-being in the Black community and where others have historically suffered from underinvestment
NSF’s values demand that our service to the public reflects respect and equality, and we commit to continue learning and doing even more to be an effective leader in public sleep health. We are charged to do our part to translate science and knowledge into advocacy and action that can bring change.
About the National Sleep Foundation
National Sleep Foundation (NSF) is a 501(c)3 nonprofit corporation dedicated to improving health and well-being through sleep education and advocacy. Founded in 1990, the NSF is committed to advancing excellence in sleep health theory, research and practice.
theNSF.org │SleepHealthJournal.org
The National Sleep Foundation (NSF) celebrates the life and legacy of Dr. William C. Dement. It is fitting that our friend Bill passed peacefully in his sleep, in the early morning hours of June 17, 2020. Bill’s pioneering and expansive work touched millions of people around the globe, and he received NSF’s inaugural Lifetime Achievement Award in 2001.
His contributions to the sleep field began as a medical student at the University of Chicago where he helped discover the link between dreaming and Rapid Eye Movement (REM) Sleep. He coined the terms REM and NREM sleep which are now universally known. After completing both his MD and PhD degrees, Bill first went to New York City where he discovered the link between sleep onset REM periods and narcolepsy, among other groundbreaking work. He then relocated to Stanford University where he established the first successful medical clinic devoted to sleep disorders. Bill worked alongside Dr. Christian Guilleminault to establish the clinical specialty of sleep medicine, including helping to create the first medical journal devoted to the field, Sleep. He also created the first university course devoted to the topic, Sleep and Dreams, which became the most popular course in Stanford history. Bill was a renaissance man, who as an accomplished upright bass player was instrumental in helping establish the jazz program at Stanford. Bill also was active in social justice on campus.
Among Bill’s many scholarly accomplishments were his contributions to a distinctive body of literature including authorship of hundreds of scientific publications, co-authorship of the authoritative textbook in sleep medicine Principles and Practice of Sleep Medicine, and authorship of the national bestseller The Promise of Sleep. He will be known and celebrated throughout the world as one of the founders and legends in the field. A tribute to Bill was previously produced by Stanford University in commemoration of his 80th birthday and 45 years of service to the university. Importantly, perhaps the greatest part of Bill’s legacy will be his devotion to and tireless work raising awareness in the general public and in government about the importance of sleep health. Bill Dement’s vision is at the core of NSF’s mission and commitment to improving sleep health and well-being, and we are grateful to have known Bill and worked with him.
About the National Sleep Foundation
National Sleep Foundation (NSF) is a 501(c)3 nonprofit corporation dedicated to improving health and well-being through sleep education and advocacy. Founded in 1990, the NSF is committed to advancing excellence in sleep health theory, research and practice.
theNSF.org │SleepHealthJournal.org
Washington, D.C. (June 15, 2020): The National Sleep Foundation (NSF) has named John Lopos as its new CEO. Mr. Lopos’ appointment is effective immediately.
“On behalf of the Board of Directors, I am excited knowing John will guide the NSF into its next period of leading the ongoing transformation in public sleep health and well-being,” said Richard Bogan, MD, FCCP and Chairman of the Board. “He has a dynamic background and strong executive insights, with a track record in organizational and healthcare strategy. His demonstrated advocacy and service to public health will keep the NSF highly relevant and help us set new standards while we achieve our ambitious mission.”
With nearly 30 years of diverse experience across multiple healthcare and non-profit organizations, Mr. Lopos has longstanding ties to the sleep health community, including his relationship with the NSF for the past 17 years. Most recently, he served for 8 years as an NSF Director, having been active on several task forces and committees including Development, Public Awareness, Compensation, and Finance. He also has been part of the organization’s advocacy on Capitol Hill for the past several years.
“Marking our 30th anniversary, the NSF is at our strongest point yet. We are on a trajectory to make an even greater impact on what the public, policymakers, and industry understand and do to connect the fundamental importance of sleep to overall health and lifestyle,” said
Mr. Lopos. “I am looking forward to using my experiences and professional purpose at a ground-breaking institution I have known for more than half its life, and I will be focusing on an area of public health to which I am deeply committed.”
About the National Sleep Foundation
National Sleep Foundation (NSF) is a 501(c)3 nonprofit corporation dedicated to improving health and well-being through sleep education and advocacy. Founded in 1990, the NSF is committed to advancing excellence in sleep health theory, research and practice.
theNSF.org │SleepHealthJournal.org
For Immediate Release
Contact: NSF Communications
703-243-1753
scorkett@thensf.org
Washington, D.C. (June 12, 2020): National Sleep Foundation (NSF) and Health Forward Media reached an agreement in December 2019 to transition the ownership, operating control and day-to-day management of the sleep.org and sleepfoundation.org web properties, with content licensed from NSF to Health Forward Media.
This change will allow these two highly-trafficked and award-winning platforms to expand the reach of NSF’s public education mission to promote public awareness and understanding of sleep-related issues, using next-generation technology. Visitors can continue to access NSF’s award-winning content on these sites, as well as at NSF-operated websites, theNSF.org, drowsydriving.org, and sleepforkids.org.
In addition, NSF continues to develop rich sleep health content for digital, print, and broadcast formats.
—
About the National Sleep Foundation
National Sleep Foundation (NSF) is a 501(c)3 nonprofit corporation dedicated to improving health and well-being through sleep education and advocacy. Founded in 1990, the NSF is committed to advancing excellence in sleep health theory, research and practice.
theNSF.org │SleepHealthJournal.org
For Immediate Release
Contact: Stephanie Corkett
703-243-1753
scorkett@thensf.org
Sleep in a Time of Pandemic: A Position Statement from the National Sleep Foundation
Washington, D.C. (May 19, 2020) – National Sleep Foundation (NSF) urges the public to follow healthy sleep habits and keep regular sleep schedules during the COVID-19 crisis to prevent circadian rhythm changes that can worsen sleep. With the global pandemic and the ever-changing news alerts, many people are experiencing high levels of stress and anxiety, which are linked with poor sleep health. Now more than ever, we need the restorative power of sleep.
Our 24-hour wake and sleep times are strongly influenced by our circadian biology. The circadian system that controls the rhythms of our lives is highly sensitive to changes in our schedules, activities, the timing of meals, and light exposure. During this massive disruption to our lives, we should all pay special attention to keeping our schedules and biological clock as consistent as possible to preserve normal circadian biology.
In order to keep our circadian rhythm intact and best able to help us maintain good sleep, we should wake up and go to bed at consistent times every day, follow a regular exercise regimen, and go outside daily to get some fresh air and sunlight.
Take this abnormal situation and turn it into an opportunity to see how your daily activities impact your sleep health. You can improve your sleep quality in the long term by being mindful of your sleep habits and tracking your sleep. If you have a smartwatch or fitness tracker, use the sleep tracker function to monitor your sleep to determine the amount you need each night to wake up fully refreshed. If you do not have a way to electronically track your sleep, keep a journal for two weeks to record the time you went to sleep, got up for the day, and how you felt when you woke up in the morning.
If stress from COVID-19 is affecting your sleep, the National Sleep Foundation has information on how to get a better night’s sleep. The National Sleep Foundation gratefully acknowledges Drs. Thomas Roth and Andrew Krystal for developing this Position Statement.
This statement was approved by the National Sleep Foundation Board of Directors on May 11, 2020.
About the National Sleep Foundation
National Sleep Foundation (NSF) is a 501(c)3 nonprofit corporation dedicated to improving health and well-being through sleep education and advocacy. Founded in 1990, the NSF is committed to advancing excellence in sleep health theory, research and practice.
theNSF.org │SleepHealthJournal.org
National Sleep Foundation CEO David Cloud announced he will step down at the end of the year after leading the organization for 13 years. During this time, NSF transformed its programs and websites, pioneered sleep technology standards, developed its public sleep guidelines, and launched an award-winning journal. These efforts helped NSF propel sleep health into the mainstream.
Mr. Cloud said, “Clearly communicating the relationship between sleep and human health set the stage for the explosive growth in sleep health products and services we are witnessing today. It has been an honor to be a part of that change and watch it come together. The next phase promises to be no less exciting, but it is also a natural time for me to step aside.”
Cloud will be working with the NSF throughout the transition. After careers with the American Medical Association and as the owner of an association management company, Cloud indicated he is weighing private and public sector opportunities.
About the National Sleep Foundation
National Sleep Foundation (NSF) is a 501(c)3 nonprofit corporation dedicated to improving health and well-being through sleep education and advocacy. Founded in 1990, the NSF is committed to advancing excellence in sleep health theory, research and practice.
theNSF.org │SleepHealthJournal.org
Contact: Stephanie Corkett
703.243.1753
scorkett@thensf.org
The National Sleep Foundation’s 2020 Sleep in America® Poll Shows Alarming Level of Sleepiness and Low Levels of Action
Washington, D.C. (March 7, 2020) – The National Sleep Foundation’s (NSF) annual Sleep in America® poll shows Americans feel sleepy on average three times a week, with 62% trying to “shake it off” as their primary response.
“I have patients in my office every day who can’t understand why they are always so sleepy,” said Dr. Paul Doghramji, physician at the Collegeville Family Practice. “It’s concerning to see so many sleepy Americans with no plan other than to shake it off” Dr. Doghramji added.
Those who feel sleepy five to seven days a week report especially high rates of irritability (52 percent), headaches (40 percent), and feeling unwell (34 percent). “Frequently, friends and family notice the effects of sleepiness including changes in mood and irritability before you do,” said Dr. Temitayo Oyegbile-Chidi, Pediatric Neurologist, Georgetown University Hospital.
The Sleep in America poll found when people feel sleepy, more Americans say it’s generally because they’re not sleeping well enough (55 percent) as opposed to not having enough time to sleep (44 percent). “Not getting the restorative benefit of sleep when you give yourself enough time for sleep could be a sign of other issues and should not be ignored.” said Dr. Oyegbile-Chidi.
“These data suggest that people continue to avoid sleepiness as a symptom, but disregarding persistent sleepiness is ill-advised,” said Dr. Patrick Strollo, Professor of Medicine and Clinical and Translational Science, University of Pittsburgh. “Sleepiness isn’t normal. If you experience routine sleepiness you should address it” added Dr. Strollo.
The NSF recommends 7-9 hours of sleep for adults aged 18-64 and 7-8 hours for older adults aged 65 and over. Characteristics of a good night’s sleep include waking up feeling refreshed, alert, and able to be fully productive throughout your waking hours. The NSF’s Sleep Health Index® score – based on measures of sleep quality, sleep duration and disordered sleep – is worse among people who report having more sleepy days. In the 2020 Q1 Sleep Health Index, sleep quality, rated 64 on a scale of 0-100, was below average compared to prior Indexes.
“We know from prevalence and longitudinal data that one-third of the population is concerned over their sleepiness as it affects their lives and ability to perform their jobs,” said Dr. Maurice Ohayon, Director of the Stanford Sleep Epidemiology Research Center.
There are simple and effective sleep tips to help you get a good night’s sleep. Sticking to a sleep schedule, even on weekends, and practicing a relaxing bedtime ritual are great first steps. The easiest way to get started is to start tracking your sleep. There are many devices and apps available to help you sleep better.
About the National Sleep Foundation
National Sleep Foundation (NSF) is a 501(c)3 nonprofit corporation dedicated to improving health and well-being through sleep education and advocacy. Founded in 1990, the NSF is committed to advancing excellence in sleep health theory, research and practice.
theNSF.org │SleepHealthJournal.org
About the Sleep in America® Poll
The Sleep in America poll is the National Sleep Foundation’s premier annual review of current sleep topics. The poll was first conducted in 1991 and has been produced since 2018 by Langer Research Associates.
Daylight Saving Time starts Sunday, March 8. Changing our clocks is a practical reminder of the negative effects of sleep loss. For the last thirty years, the NSF has released its Sleep in America poll with the start of Daylight Saving Time.
The full Sleep in America poll findings, the Langer Research Associates report, including methodology, can be found at Sleep in America poll page or the Sleep Health Journal.
About the Sleep Health Index®
The Sleep Health Index is a quarterly fielded, nationally representative survey of American adults; it tracks trends and chronicles our nation’s sleep health over time.
This quarterly Sleep Health Index was administered alongside the Sleep in America poll and explored stress and sleep. For more information on the methodology, go to the Sleep Health Journal.
Contact: Stephanie Corkett
703.243.1753
scorkett@thensf.org
Washington, D.C. (March 2, 2020) – The National Sleep Foundation (NSF) prepares to launch its signature public awareness and education initiative, Sleep Awareness Week® 2020, taking place on March 8-14.
The annual Sleep Awareness Week celebrates sleep health and encourages the public to prioritize sleep to improve their overall health and well-being. The national campaign provides valuable information about the benefits of optimal sleep and how sleep affects health, well-being, and safety. NSF will launch the campaign on social media using hashtag #MySleepHealth. NSF invites the public, sleep industry and the broader health community to join in amplifying this year’s campaign messages promoting healthy sleep.
On March 7th in conjunction with Sleep Awareness Week, NSF will release the results of the 2020 Sleep in America® poll that asked Americans about their attitudes and behaviors about sleep. NSF will also release its quarterly Sleep Health Index® score based on measures of sleep quality, sleep duration and disordered sleep.
Sleep Awareness Week begins at the start of Daylight Saving Time when most Americans lose an hour of sleep. The change to Daylight Saving Time reminds us to make beneficial changes in our sleep routines to improve our sleep health.
Sleep Awareness Week is supported by unrestricted grants from Eisai, Inc. and Fisher & Paykel Healthcare. NSF produces Sleep Awareness Week, Sleep in America poll, Sleep Health Index and all educational content independently with its sleep experts.
About the National Sleep Foundation
National Sleep Foundation (NSF) is a 501(c)3 nonprofit corporation dedicated to improving health and well-being through sleep education and advocacy. Founded in 1990, the NSF is committed to advancing excellence in sleep health theory, research and practice.
theNSF.org │SleepHealthJournal.org
FOR IMMEDIATE RELEASE
nsfmedia@thensf.org
WASHINGTON, DC, February 10, 2020 – Today the National Sleep Foundation announces that Sleep Awareness Week® 2020 will take place on March 8-14.
The annual Sleep Awareness Week celebrates sleep health and encourages the public to prioritize sleep to improve their overall health and well-being. The national campaign will provide valuable information about the benefits of optimal sleep and how sleep affects health, well-being, and safety. The week begins with the release of the results of the National Sleep Foundation’s annual Sleep in America® poll. Also at that time, the National Sleep Foundation will release the results of the quarterly Sleep Health Index® and make available shareable messages, infographics, and social media posts.
“Sleep Awareness Week shines a light on the importance of sleep health,” says National Sleep Foundation CEO David Cloud. “Sleepiness is not normal. We want everyone to feel healthy and refreshed by getting the most out of their sleep.”
Sleep Awareness Week leads up to the start of Daylight Saving Time when most Americans lose an hour of sleep. The change to Daylight Saving Time reminds us to make beneficial changes in our sleep routines to improve our sleep health.
About the National Sleep Foundation
National Sleep Foundation (NSF) is a 501(c)3 nonprofit corporation dedicated to improving health and well-being through sleep education and advocacy. Founded in 1990, the NSF is committed to advancing excellence in sleep health theory, research and practice.
theNSF.org │SleepHealthJournal.org
Each year the National Sleep Foundation recognizes innovative sleep products by giving out the SleepTech Awards, the world’s first innovation awards targeted specifically at sleep technology. This year, the winners were announced at NSF’s Sleep Show, March 8-10, 2019 in Houston, TX. Check back for updates on the 2020 Award soon!
SleepTech Award Winner: The ReST Bed™
SleepTech App Award Winner: Timeshifter – The Jet Lag App®
Semi-finalists:
Beddr Sleep Tuner™
Biostrap’s Sleep Lab
BreatheSimple
ChiliPad™
Comfort Control™ Mattress
Dreamlight Pro
Embr Wave
EyeJust
GetSnooze
Inspire Therapy
Nanit Plus
Nasalaid
Night Owl®
Oura
Sleep by Headspace
Sleep Equ
Sleep-A-Board
SleepPhones® Effortless™
SleepScore App
Smart Nora
Somnox Sleep Robot
SonicTonic
Sound + Sleep SE
Tatch™ Sleep Patch
The ReST Bed™
Timeshifter – The Jet Lag App®
Tranquilo Mat
URGONight
Read the 2019 Award Press Release
March 21, 2019
ReST® (Responsive Surface Technology) Performance and Timeshifter® Win National Sleep Foundation SleepTech® Awards
The National Sleep Foundation (NSF) announces the winners of the 2019 SleepTech Awards. These awards recognize innovative sleep technology companies. Twenty-eight semi-finalists pitched their product to a panel of judges in front of a live audience at Sleep Show® in Houston, Texas on March 9th. Five finalists were selected from this group.
The ReST Bed™, which senses a sleeper’s position and makes automatic real-time adjustments, won the 2019 SleepTech Award. Timeshifter – The Jet Lag App® based on sleep and circadian neuroscience research won the 2019 SleepTech App Award.
Congratulations to ReST, Timeshifter, and all of the semi-finalists! NSF can’t wait to showcase more exciting innovations next year.
To learn more or receive application updates, please contact education@thensf.org.
In 2017, the National Sleep Foundation launched the world’s first innovation award for sleep technology. With so many companies developing exciting new technologies, NSF believes it is time to formally recognize these innovations.
The 18 unique semi-finalists pitched their products to an expert panel of judges at the third annual SleepTech® Summit co-located with the 2017 Health 2.0 Fall Conference. Happiest Baby’s SNOO Smart Sleeper was named the winner!
SNOO features adjustable and automated rocking motions, white noise generation, and a variety of safety and comfort features with the aim of helping babies sleep longer and better The award was presented to Dr. Harvey Karp, Happiest Baby’s Founder and CEO.
Congratulations to Happiest Baby and all of the semi-finalists! NSF is already looking forward to the innovations that 2018’s entrants will bring to the next SleepTech® Award. To learn more or receive award application updates, please contact us at education@thensf.org.
